The Critical Role of Vision in Early Development
Vision plays a central role in early childhood development, influencing motor coordination, cognitive growth, communication, and social-emotional well-being. From infancy, visual input shapes how children engage with their environment and acquire foundational skills. Yet vision screening for children under age three remains underutilized and often overlooked across public health and early childhood systems (Hartmann et al., 2019). There is no national mandate requiring screening before age three, and many healthcare providers report limited tools or guidance for detecting vision issues in nonverbal children (Donahue et al., 2016). During the first three years of life—a period of rapid visual and neurological development—the brain’s visual pathways are especially plastic and responsive to sensory input (Levi, 2013).
If disrupted by conditions such as refractive error, strabismus, or congenital cataracts, this development can be permanently impaired (Holmes et al., 2011). Despite the critical nature of early vision, many disorders go undetected until preschool or later, missing the optimal window for intervention (American Academy of Pediatrics [AAP], 2021). The Birth-to-3 Years Vision Screening Program was created to address this gap through developmentally appropriate, equity-centered, and proactive screening. It uniquely integrates screening into multiple systems of care—including early intervention (IDEA Part C), pediatric primary care, and public health—and employs a multimodal approach using parental input, clinical observation, and instrument-based tools. This model reflects a shift from reactive treatment to early identification, ensuring timely detection, referral, and support for children at risk of visual impairment. This article is intended for pediatric professionals, early interventionists, public health leaders, and policymakers seeking evidence-based strategies to close screening gaps, improve developmental outcomes, and reduce disparities in pediatric eye care.
Scientific Rationale
The visual cortex and associated neural pathways develop rapidly during the first three years of life—a critical period marked by experience-dependent plasticity, in which the brain organizes itself in response to visual input (Levi, 2013). When visual stimuli are disrupted by conditions such as refractive error, strabismus, or congenital cataracts, these neural pathways may fail to form properly, resulting in amblyopia or other permanent impairments. Neuroscientific research confirms that the visual system is most malleable during this early window, and intervention is most effective when initiated before age two (Holmes et al., 2011).
For example, strabismus treatment yields better outcomes when started before 24 months, and congenital cataracts must be addressed within the first weeks of life to preserve vision (AAP, 2021). These conditions are often subtle or asymptomatic, making them difficult to detect without formal screening. If left uncorrected, early visual impairment can delay language development, hinder motor skills, impair social-emotional growth, and contribute to long-term learning challenges (Miller et al., 2014). These ripple effects underscore the urgency of universal vision screening before age three, when intervention can have the most profound and lasting impact.
Why Vision Screening Is Urgently Needed in the Birth-to-3 Population
The first three years of life represent a period of intense visual and neurological development. During this time, the brain's visual pathways are highly plastic and responsive to sensory input. Disorders such as strabismus, congenital cataracts, cortical visual impairments, or uncorrected refractive error can interfere with synaptic development and lead to amblyopia—permanent vision loss due to disuse—even if the eye appears structurally normal (Levi,2013). Because these problems are often asymptomatic and difficult for families to detect, the absence of routine screening places children at high risk. Delays in treatment not only affect visual acuity but also contribute to challenges in school readiness, motor coordination, attention, and language development.
Currently, the U.S. Preventive Services Task Force (USPSTF, 2017) recommends screening for amblyopia starting at age three. However, this leaves a critical developmental window unaddressed. The Birth-to-3 program fills this gap by offering timely identification and referral during the period when intervention is most effective.
What Makes the Birth-to-3 Program Unique?
Several features distinguish this program:
- Age focus: Unlike typical preschool screening, the program targets children from birth to age three—when vision disorders can be most damaging and most reversible.
- Multimodal approach: Combines parental questionnaires, clinical observations, and instrument-based tools.
- Cross-system integration: Operates within early intervention (IDEA Part C), pediatric primary care (Bright Futures well-child visits), and public health (e.g., mobile clinics).
- Commitment to equity: Targets underserved populations through community-based outreach, culturally responsive tools, and accessible service models.
By leveraging multiple access points and screening strategies, the program improves both reach and effectiveness.
Program Structure and Integration
The Birth-to-3 Years Vision Screening Program rests on five guiding objectives:
- Early Identification of overt and subtle vision issues.
- Timely Referral pathways to pediatric eye-care professionals.
- Family Education and Support throughout screening and treatment.
- Ongoing Monitoring of visual development through early childhood.
- Equity and Access across socioeconomic, racial, and geographic boundaries.
The program is typically embedded in early intervention systems (e.g., IDEA Part C), pediatric primary care, and public health initiatives. This integration enables consistent screening during routine health visits and early childhood program enrollment. Embedding vision screening into existing structures minimizes burden and maximizes reach.
Milestones in Infant and Toddler Vision
Tracking developmental milestones is essential for effective screening:
- 0–1 month: light sensitivity, blinking to bright light
- 2–3 months: eye tracking, social smiling
- 4–6 months: binocular vision, eye-hand coordination
- 7–12 months: depth perception, facial recognition
- 12–24 months: smooth pursuit movements, object permanence
- 24–36 months: visual memory, imitation of actions
While some variability in development is normal, significant deviations from these benchmarks may indicate vision concerns that warrant follow-up.
Screening Components
Parental Questionnaires
Caregiver-reported tools, such as the Parent Questionnaire for Infant Vision (PQIV), offer valuable insights into a child's visual behavior at home. These instruments assess blinking, facial recognition, light sensitivity, and tracking—critical indicators in infants and toddlers who cannot reliably participate in formal testing. To be effective, questionnaires must be culturally sensitive, linguistically accessible, and supported with clear examples or guidance. Parents are often the first to notice subtle signs, and structured tools help transform these observations into actionable data.
Clinical Observations
Pediatricians and trained screeners conduct in-office assessments including red-reflex testing, cover-uncover tests, pupil reactivity, and fixation-tracking evaluations. These methods can detect cataracts, strabismus, neurological anomalies, and other alignment issues. Accurate interpretation depends on proper training and an understanding of age-appropriate visual responses.
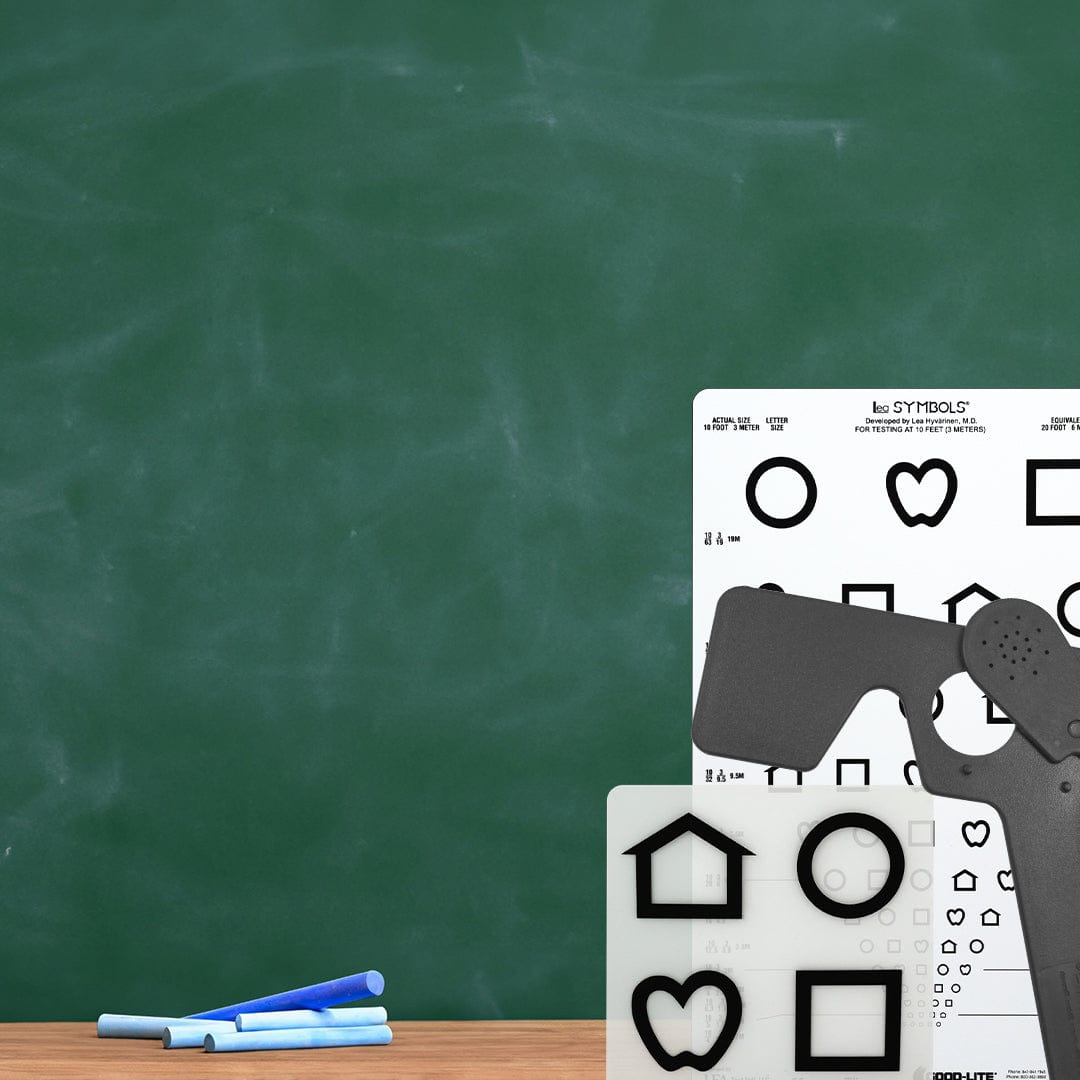
Instrument-Based Screening
Handheld autorefractors and photorefraction devices provide objective, non-invasive assessments of refractive error and structural anomalies. These tools are highly effective in toddlers; however, in infants under 12 months, limited fixation time and physiological hyperopia may result in higher false-positive rates (Donahue et al., 2016). Current professional guidelines, including those from the American Academy of Pediatrics, recommend using instrument-based tools only after one year of age and in combination with clinical observations and caregiver input to improve accuracy and reliability. Instrument-based screening is most powerful when embedded in a broader clinical and family-centered context.
Multidisciplinary Roles
The Birth-to-3 program relies on a team-based model:
- Pediatricians initiate screening and guide families to follow-up care.
- Early interventionists observe vision use during daily routines and support family engagement.
- Teachers of the Visually Impaired (TVIs) provide adapted materials and developmental support.
- Orientation and Mobility Specialists address spatial awareness and safe navigation.
- Optometrists and Ophthalmologists conduct diagnostic evaluations and provide treatment including glasses, surgery, or therapy.
Collaboration across these disciplines ensures timely identification, follow-through, and individualized intervention for each child.
Embedding in Systems of Care
Integration with established service frameworks enhances reach and efficiency:
- IDEA Part C mandates vision screening within 45 days of program enrollment.
- Early Head Start reaches families with limited access to pediatric care.
- The Medical Home Model (American Academy of Pediatrics) calls for vision screening at every well-child visit.
- Mobile Clinics extend access to rural and underserved communities.
Such cross-sector approaches allow the program to meet families where they are.
Challenges and Solutions
While the benefits are clear, several implementation challenges persist:
- Standardization: Variation in tools, procedures, and referral thresholds across jurisdictions can lead to inconsistent results.
- Access: Shortages of pediatric eye care providers in rural and low-income communities delay follow-up and treatment.
- Language and Literacy Barriers: Families may struggle to understand screening outcomes or access care, particularly if materials are not culturally responsive.
- Sustainability: Funding limitations threaten the longevity of many programs, especially those dependent on grants or unbillable services.
Solutions include national screening standards, telehealth consultations, translation services, mobile units, and policy advocacy for insurance reimbursement and public investment. Addressing these barriers is essential for scaling early vision screening equitably.
Evidence Base and Future Directions
Longitudinal studies show that children treated early for visual impairments demonstrate better developmental outcomes and reduced need for special education (Hartmann et al., 2019). Cost-effectiveness research further validates investment in early screening, with reduced long-term costs for education, health care, and lost productivity (Miller et al., 2014).
Emerging innovations include:
- AI-enabled screening apps that use smartphone cameras to analyze red reflex or detect misalignment
- Remote monitoring tools that allow families and providers to track visual development over time
- Wearable devices that assess gaze behavior and visual engagement
These advances will expand screening access and accuracy, particularly in underserved settings.
Call for Universal Implementation
Currently, only half of U.S. states mandate preschool vision screening, and even fewer require screening under age three (USPSTF, 2017). The U.S. Preventive Services Task Force recommends amblyopia screening beginning at age three, despite growing evidence for earlier identification.
The Birth-to-3 program’s results—showing over 95% sensitivity and strong predictive validity—make a compelling case for national adoption. Scaling the program would:
- Standardize protocols across all jurisdictions
- Integrate services with early childhood systems
- Address equity through community-based outreach and culturally competent practices
- Build infrastructure for tracking outcomes and continuous improvement
Such a model promotes consistency, reduces disparities, and ensures no child falls through the cracks.
How Good-Lite Digital Can Support Early Screening Models
While comprehensive diagnosis belongs in clinical settings, early identification relies on accessible, standardized screening across systems. Tools within the Good-Lite Digital ecosystem—including GLD-Vision® and Good-Lite Studio®—offer developmentally appropriate, standardized workflows that complement early intervention systems and pediatric primary care. These platforms support:
- secure documentation
- family notifications
- referral tracking
- data continuity across programs
Good-Lite’s full catalog of pediatric tools (store.good-lite.com) further supports clinicians with child-appropriate stimuli, fixation targets, and vision development resources.
Conclusion
Vision is a critical developmental domain, and the first three years of life offer a unique window to identify and treat disorders before they cause lasting harm. The Birth-to-3 Years Vision Screening Program provides a replicable model for proactive, equitable pediatric vision care. With growing scientific evidence, technological advances, and systems-level integration, universal early vision screening is both feasible and urgent.
Investing in this foundational component of child development ensures that all children—regardless of background—enter school ready to see, learn, and thrive.
References
- American Academy of Pediatrics. (2021). Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics, 147(1), e2020029074.
- Donahue, S. P., Baker, C. N., & Committee on Practice and Ambulatory Medicine, Section on Ophthalmology. (2016). Procedures for the evaluation of the visual system by pediatricians. Pediatrics, 137(1), e20153597.
- Hartmann, E. E., Block, S. S., Wallace, D. K., & Morse, C. L. (2019). Vision screening for children younger than age 3 years: A systematic review. Preventive Medicine, 118, 228–237.
- Holmes, J. M., Clarke, M. P., & Powell, C. (2011). The importance of early treatment for amblyopia. Ophthalmology, 118(5), 1230–1234.
- Levi, D. M. (2013). Linking assumptions in amblyopia. Visual Neuroscience, 30(5–6), 277–287.
- Miller, J. M., Lessin, H. R., & American Academy of Pediatrics. (2014). Vision screening in the pediatric office setting. Pediatrics, 134(1), e178–e182.
- U.S. Preventive Services Task Force. (2017). Vision screening in children aged 6 months to 5 years: Recommendation statement. JAMA, 318(9), 836–844.