Table of contents
Innovation is transforming eye care delivery. Telehealth platforms, AI-assisted imaging, and digital screening technologies are expanding access and improving workflow efficiency. These advancements have undeniable value. Yet even as technology reshapes clinical systems, one foundational principle remains unchanged: diagnostic accuracy depends on comprehensive evaluation.
A recent Editors’ Choice article from the American Academy of Ophthalmology highlights this reality. The research suggests that in-person eye examinations can improve diagnostic accuracy compared to limited or remote assessments in certain contexts. The findings do not dismiss telemedicine. Rather, they clarify the clinical role of comprehensive in-person exams within a modern care model.
Understanding the Difference Between Screening and Diagnosis
Screening programs play a critical role in early detection. They identify individuals at risk, prioritize referrals, and increase system efficiency. However, screening is not the same as diagnosis. Screening is designed to detect potential abnormalities. Diagnosis requires confirmation, differentiation, and treatment planning. That process demands a higher level of clinical accuracy.
In-person examinations allow clinicians to perform slit-lamp biomicroscopy, dilated retinal evaluation, intraocular pressure measurement, and detailed optic nerve assessment. These components contribute directly to diagnostic accuracy by providing layered clinical information that cannot always be captured through image transmission alone.
For example, subtle anterior segment findings, mild optic nerve head asymmetry, or early retinal pathology may only become apparent during direct examination. In these situations, physical presence strengthens clinical confidence and reduces the risk of misclassification.
Why Comprehensive Evaluation Improves Accuracy
Clinical decision-making is rarely binary. Many ocular conditions share overlapping features. Distinguishing between inflammatory, vascular, glaucomatous, or neuro-ophthalmic causes often depends on contextual interpretation. In-person evaluation enhances diagnostic accuracy by allowing clinicians to adjust examination strategy in real time.
Dynamic Clinical Reasoning
When a clinician observes a patient directly, they are not limited to pre-captured data points. They can ask additional questions, repeat tests, examine peripheral fields, or adjust magnification and lighting. This dynamic reasoning improves diagnostic accuracy, particularly in complex or atypical presentations.
Subtle Findings That Influence Outcomes
Early glaucoma changes, mild corneal edema, subtle uveitis, or peripheral retinal tears may not always be obvious in remote imaging. These findings can influence management decisions significantly. The AAO article emphasizes that in-person exams may lead to more precise diagnosis, reinforcing that physical examination remains a central pillar of quality care.
Accuracy in diagnosis directly impacts treatment decisions, monitoring intervals, and patient outcomes. A missed finding does not merely delay care; it may alter long-term visual prognosis.

Balancing Access and Accuracy in Modern Eye Care
Expanding access to care is a priority across global health systems. Telehealth and digital tools improve reach, especially in rural or underserved regions. Portable screening systems help identify patients earlier and streamline referrals. These tools support scalability and efficiency.
However, access alone does not guarantee diagnostic accuracy. A balanced model recognizes that screening and remote triage enhance reach, while comprehensive in-person evaluation strengthens diagnostic precision. The goal is integration, not substitution.
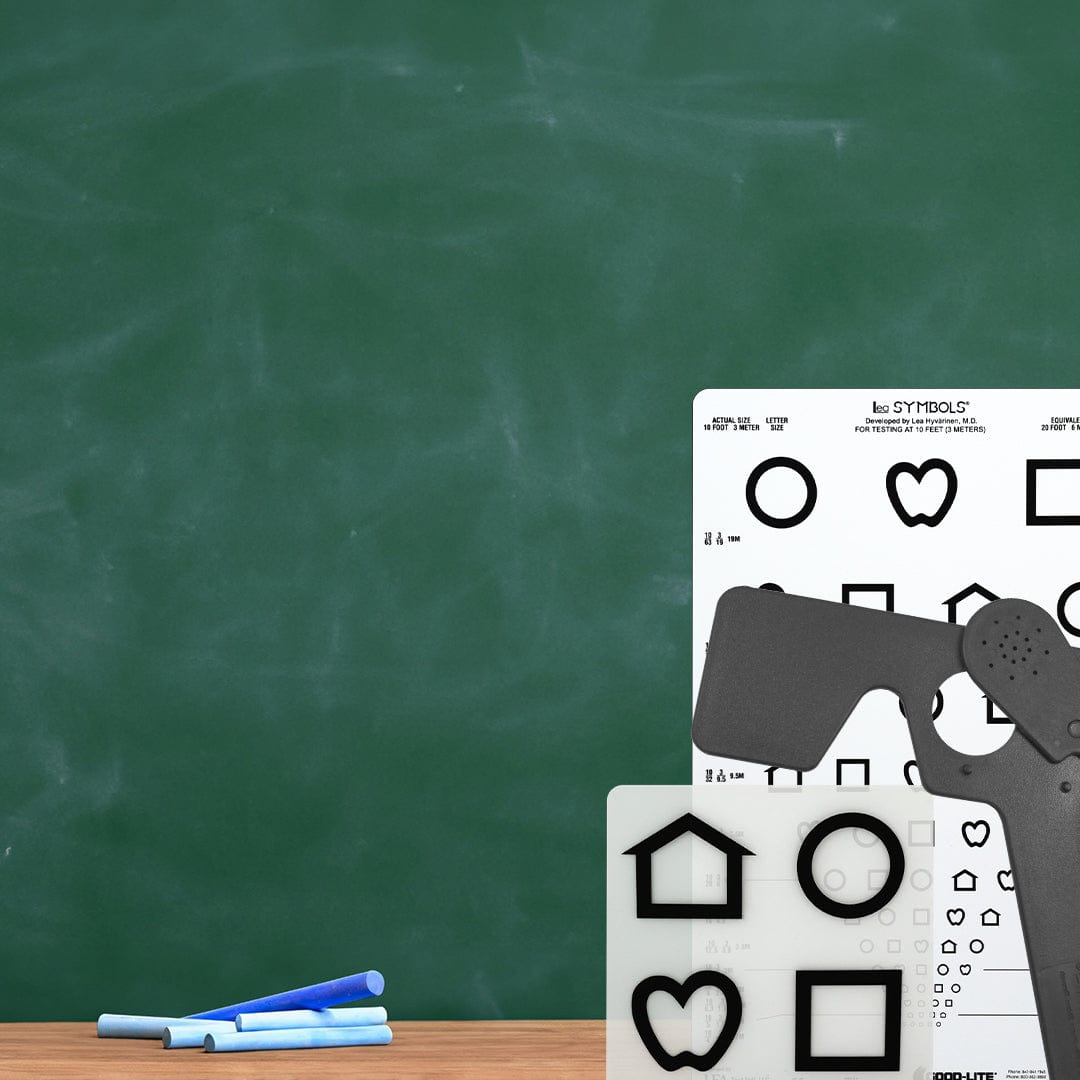
For example, structured screening platforms such as GLD-Vision support standardized vision assessment workflows. In educational or community settings, these systems improve detection rates and referral efficiency. Yet once risk is identified, the pathway must include access to comprehensive clinical evaluation to preserve diagnostic accuracy.
Implications for Health Systems and Clinical Leadership
For clinicians, this research reinforces the importance of comprehensive evaluation in maintaining professional standards. Diagnostic accuracy is not simply about identifying disease; it is about differentiating between possible causes and confirming findings with confidence.
For health systems, the findings suggest that care models should integrate digital screening with structured referral pathways. Designing systems that connect early detection with in-person evaluation protects both patient safety and clinical integrity.
Designing Integrated Care Pathways
Effective care models align screening, telehealth triage, and in-person examination into a cohesive structure. Screening identifies risk. Telehealth facilitates monitoring and accessibility. Comprehensive examination confirms diagnosis. When these components function together, both access and diagnostic accuracy improve.
Health systems that prioritize only one component risk imbalance. Overreliance on remote evaluation may compromise diagnostic confidence. Ignoring digital tools may limit access unnecessarily. Sustainable leadership requires clarity about where each modality adds value.
Protecting Diagnostic Standards in a Changing Landscape
The modernization of eye care is a sign of progress. AI tools assist in pattern recognition. Digital imaging supports documentation and consultation. Portable screening increases community reach. These developments should be embraced.
At the same time, protecting diagnostic accuracy remains non-negotiable. In-person examination allows clinicians to synthesize findings holistically. It reinforces accountability and strengthens decision-making in complex cases.
The AAO Editors’ Choice discussion serves as a timely reminder: technology enhances care, but comprehensive evaluation remains fundamental to clinical accuracy. As the profession evolves, maintaining this balance will define the quality of future eye care systems.
Ultimately, innovation and tradition are not opposing forces. They are complementary tools. When screening expands access and in-person exams protect diagnostic accuracy, patients benefit from both reach and precision.