Table of contents
Myopia is no longer viewed as a simple refractive inconvenience. It is a growing global public health concern with long-term implications for ocular health, visual performance, and healthcare systems. As prevalence continues to rise worldwide, particularly among children and adolescents, the conversation has shifted from correction to prevention, monitoring, and long-term risk management. Recent research published in Scientific Reports reinforces that effective management of myopia depends not only on intervention strategies, but also on diagnostic precision and measurement reliability.
The study examines how measurement variability and diagnostic thresholds influence long-term monitoring decisions. While myopia progression is often tracked through changes in spherical equivalent refraction or axial length, even small inconsistencies in measurement can alter interpretation. Over time, those variations affect treatment decisions, risk assessment, and clinical confidence.
Why Diagnostic Precision Matters in Myopia Monitoring
In early-stage myopia, small shifts in refractive error may signal accelerating progression. Clinicians rely on consistent, reproducible measurements to determine whether progression is stable, slowing, or worsening. The Scientific Reports paper emphasizes that variability in measurement techniques can influence how progression trends are interpreted, particularly when changes are subtle.
As the authors note, “measurement precision plays a critical role in longitudinal assessment,” highlighting the importance of minimizing noise when monitoring refractive change. This is especially relevant in pediatric populations, where small increments in axial elongation may precede significant refractive shifts.
In practical terms, this means that the tools and protocols used to assess myopia must be standardized. Differences in device calibration, lighting conditions, fixation stability, and examiner technique can all introduce variability. Over multiple visits, that variability can compound.
“As reported in Scientific Reports, high measurement precision is essential for reliable longitudinal assessment, particularly when monitoring refractive change over time.”
Measurement Variability and Clinical Interpretation
One of the central themes of the study is the distinction between biological change and measurement noise. When clinicians evaluate myopia progression, they must determine whether a shift represents true axial elongation or simply normal testing variation. Without high measurement reliability, distinguishing between these becomes difficult.
This is particularly relevant when implementing myopia control interventions. Whether prescribing specialty lenses, orthokeratology, or pharmacological strategies, clinicians need confidence that observed changes reflect treatment response rather than statistical fluctuation. Diagnostic precision directly influences clinical decisions.

Myopia as a Long-Term Risk Factor
Beyond refractive inconvenience, progressive myopia increases the risk of retinal detachment, myopic maculopathy, and other sight-threatening conditions. The long-term risks associated with progressive myopia, including retinal detachment and myopic maculopathy, are well documented in epidemiological literature such as reports from the World Health Organization’s World Report on Vision.
Early detection and accurate monitoring are therefore not cosmetic goals—they are preventive strategies. The Scientific Reports findings reinforce that small inaccuracies early in monitoring may influence long-term risk trajectories. Because myopia progression often accelerates during childhood and adolescence, longitudinal tracking must be both sensitive and reliable. A system that overestimates change may trigger unnecessary intervention. A system that underestimates progression may delay needed treatment.
This balance between sensitivity and specificity is central to responsible myopia management. The study underscores the importance of defining thresholds carefully and validating diagnostic methods rigorously.
Standardization Across Devices and Settings
Another important consideration raised in the research is consistency across diagnostic devices. Axial length measurement, autorefraction, and subjective refraction may not always align perfectly. If monitoring protocols vary between clinics or even between visits, longitudinal tracking of myopia becomes less dependable.
Standardized protocols reduce this variability. Repeating measurements under similar conditions, using calibrated instruments, and applying consistent analysis criteria strengthens interpretability. The study highlights that methodological rigor enhances the reliability of longitudinal myopia research and, by extension, clinical care.
Implications for Screening and Early Detection
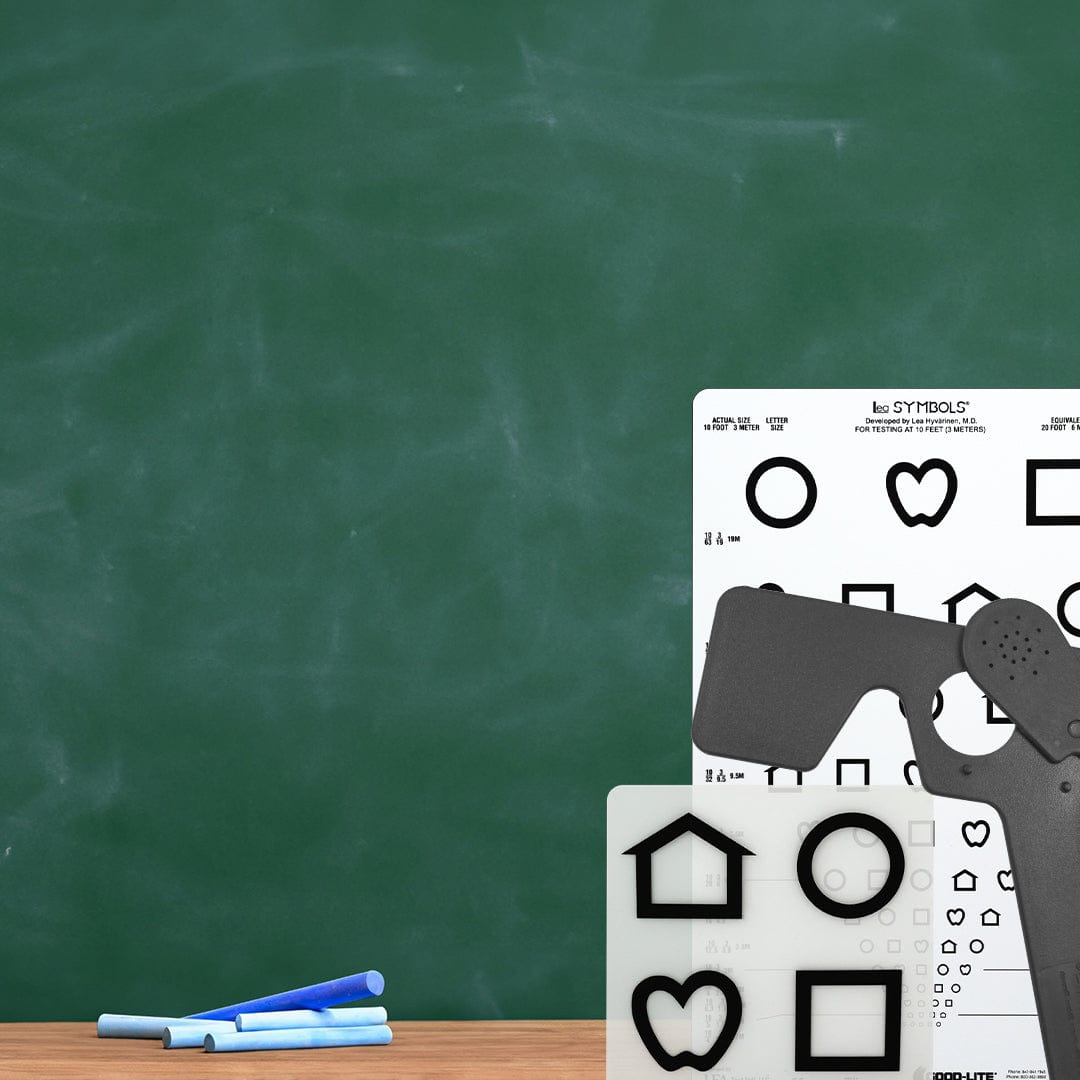
While the paper focuses on diagnostic precision, its implications extend to screening environments. Detecting early myopia in school-based or community programs depends on reliable baseline assessments. Screening tools must balance accessibility with accuracy.
Inconsistent screening methods may miss early refractive shifts or over-identify transient refractive states. For systems aiming to detect myopia early, especially in growing populations, measurement consistency becomes foundational.
This is where structured, evidence-based screening protocols matter. Screening does not replace comprehensive eye examination, but it establishes the initial reference point. Without a dependable baseline, monitoring progression becomes more difficult.
Evidence-Based Myopia Management Requires Strong Data
As global myopia prevalence increases, clinical and public health strategies must be grounded in reproducible data. Interventions are only as effective as the monitoring systems used to evaluate them. The Scientific Reports findings reinforce that careful methodological design improves both research validity and patient outcomes.
For clinicians, this means prioritizing measurement reliability when selecting tools and establishing follow-up protocols. For researchers, it underscores the importance of clearly defining endpoints and minimizing variability. For screening programs, it highlights the need for validated equipment and standardized workflows.
At Good-Lite, evidence-based vision screening has long centered on consistency and validated methodology. As conversations around myopia expand, the emphasis on precision aligns with broader clinical priorities: detect early, monitor accurately, and intervene responsibly.
Conclusion
The Scientific Reports study contributes to a growing body of literature emphasizing that myopia management is not simply about identifying refractive error. It is about ensuring that diagnostic tools are precise enough to detect meaningful change over time. Small measurement inconsistencies may appear negligible in isolation, but across years of monitoring, they shape clinical trajectories.
As myopia continues to affect larger segments of the global population, the importance of reliable, standardized, and validated diagnostic systems becomes increasingly clear. Measurement precision is not a technical detail—it is the foundation of responsible long-term care.
Source: Scientific Reports (Nature Portfolio), 2026.